Abstract
Background Diffuse large B-cell lymphoma (DLBCL) is the second most common lymphoid malignancy in the adolescent and young adults (AYA) age group defined as young people between 15 to 39 years of age (Blum et al, BJH, 2018) and AYA patients with DLBCL have better 5-year(yr) relative survival than adult patients with DLBCL. While outcomes of DLBCL in the United States have improved significantly over the years, significant racial disparities remain. Black patients with DLBCL present at younger age, more advanced stage, and have inferior survival (Shenoy et al, Cancer, 2011). We sought to determine whether similar racial disparities exist in AYA-DLBCL and analyze the specific factors associated with survival disparities in this population.
Methods The surveillance, epidemiology and end-result (SEER) registry 2019 research plus database was utilized to assess the survival outcomes and predictors of survival in AYA population diagnosed with DLBCL non-specified (NOS). Log-rank cox proportional hazards regression was used to analyze factors associated with the survival. Both univariate and multivariate analysis were performed. All analysis were adjusted to confounding factors. Wilcoxon rank sum test, Pearson chi square test were used to compare baseline characteristics. RStudio 2022.02.3+492 was used and a two-sided p-value <0.05 was considered significant.
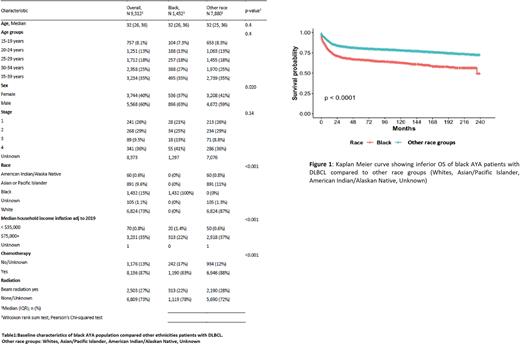
Results A total of 9312 AYA-DLBCL patients were identified in the SEER database between 2000-2019. Baseline characteristics were as follows- gender: male 60%, female 40%; age distribution: 15yr-19yr 8%, 20-24yr 13%, 25-29yr 18%, 30-34yr 25%, 35-39yr 35%; race distribution: white 73%, black 15%, Asian/Pacific Islander 10%, American Indian/Alaskan native 0.6%, unknown 1.1%; disease stage: I 1.2%, II 2.1%, III 2.9%, IV 3.7, unknown 90.2%. In the entire cohort, 89% patients received systemic therapy, 26.8% received RT and 11% received no therapy. Compared to other races, black patients were more likely to be men (63% vs 59%, p=0.02) and belong to low-income families (p<0.001). While a higher percentage of black patients presented with advanced stage (III/IV) disease (54% vs 44.8%), this finding was not statistically significant (p=0.14) due to lack of staging data in a majority of the cohort (90%). Notably, black patients were less likely to receive chemotherapy than other races (83% vs 88%, p<0.001). (See table 1 for baseline characteristics)
The 5-year overall survival (OS) was 78.5% in the entire cohort. Black patients had an inferior 5-year OS compared to other races (66.6% vs 80.7%, p< 0.001) (Figure 1). Older age (p<0.0001), male gender (p<0.0001), lower household income (p<0.0001) and omitting systemic chemotherapy (p<0.0001) were also associated with inferior 5-year OS. Black patients were more likely to die from DLBCL compared to other races (HR 1.94, SE 0.51, 95% CI 1.75-2.14, P<0.001). On multivariate analysis, the difference in survival between black patients and other races remained significant even after adjusting for age, gender, stage of disease, household family income and receipt of chemotherapy. Impact of year of diagnosis on outcomes and racial disparities is currently being analyzed and will be reported at the meeting.
Conclusion Black AYA-DLBCL patients had higher mortality and inferior 5-year overall survival compared to other races. The outcome disparities in black patients persisted even after adjusting for age, gender, stage, household family income, and receipt of chemotherapy. Further studies should examine differences in disease biology and other socioeconomic factors such as access to transportation, health insurance, level of healthcare education and others that may underlie the observed racial differences in presentation and outcome.
Disclosures
Torka:ADC Therapeutics: Consultancy; Genentech: Consultancy; Epizyme: Consultancy; Lilly USA: Consultancy; TG Therapeutics: Consultancy; Targeted Oncology, Physician Education Review: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal